"In 2015 the World Health Organization produced a report on non-communicable diseases, citing the four major types as most of them chronicity from clinical complexity based physico-mental health complexity; they're as follows:[14]
- Cancers
- Cardiovascular diseases, including cerebrovascular disease, heart failure, and ischemic cardiopathy
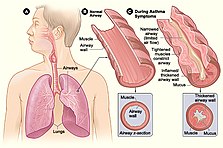
- Chronic respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD)
- Diabetes mellitus (type 1, type 2, pre-diabetes, gestational diabetes)
Other examples of chronic diseases and health conditions include:
- Alzheimer's disease
- Atrial fibrillation
- Attention deficit hyperactivity disorder
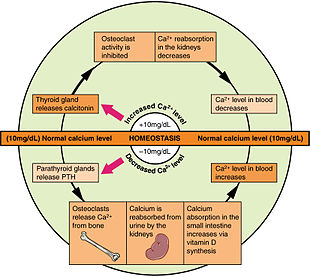
- Autoimmune diseases, such as ulcerative colitis, lupus erythematosus, Crohn's disease, coeliac disease, Hashimoto's thyroiditis, and relapsing polychondritis
- Blindness
- Cerebral palsy (all types)
- Chronic graft-versus-host disease
- Chronic hepatitis
- Chronic kidney disease
- Chronic osteoarticular diseases, such as osteoarthritis and rheumatoid arthritis
- Chronic pain syndromes, such as post-vasectomy pain syndrome and complex regional pain syndrome
- Dermatological conditions such as atopic dermatitis and psoriasis
- Deafness and hearing impairment
- Ehlers–Danlos syndrome (various types)
- Endometriosis
- Epilepsy
- Fetal alcohol spectrum disorder
- Fibromyalgia
- HIV/AIDS
- Hereditary spherocytosis
- Huntington's disease
- Hypertension
- Lyme Disease[15]
- Mental illness
- Migraines
- Multiple sclerosis
- Myalgic encephalomyelitis (a.k.a. chronic fatigue syndrome)
- Narcolepsy
- Obesity
- Osteoporosis
- Parkinson's disease
- Periodontal disease
- Polycystic Ovarian Syndrome
- Postural orthostatic tachycardia syndrome
- Sickle cell anemia and other hemoglobin disorders
- Substance Abuse Disorders
- Sleep apnea
- Tick-borne illness[16]
- Thyroid disease
- Tuberculosis
- And many more".

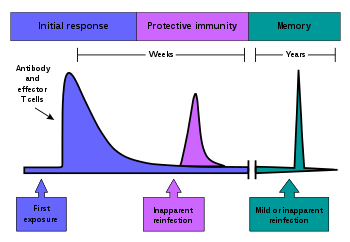
"A growing body of evidence supports that prevention is effective in reducing the effect of chronic conditions; in particular, early detection results in less severe outcomes. Clinical preventive services include screening for the existence of the disease or predisposition to its development, counseling and immunizations against infectious agents. Despite their effectiveness, the utilization of preventive services is typically lower than for regular medical services. In contrast to their apparent cost in time and money, the benefits of preventive services are not directly perceived by patient because their effects are on the long term or might be greater for society as a whole than at the individual level.[24]
Therefore, public health programs are important in educating the public, and promoting healthy lifestyles and awareness about chronic diseases. While those programs can benefit from funding at different levels (state, federal, private) their implementation is mostly in charge of local agencies and community-based organizations.[25]
Studies have shown that public health programs are effective in reducing mortality rates associated to cardiovascular disease, diabetes and cancer, but the results are somewhat heterogeneous depending on the type of condition and the type of programs involved.[26] For example, results from different approaches in cancer prevention and screening depended highly on the type of cancer.[27] The rising number of patient with chronic diseases has renewed the interest in prevention and its potential role in helping control costs. In 2008, the Trust for America's Health produced a report that estimated investing $10 per person annually in community-based programs of proven effectiveness and promoting healthy lifestyle (increase in physical activity, healthier diet and preventing tobacco use) could save more than $16 billion annually within a period of just five years.[28]
It is uncertain whether school-based policies on targeting risk factors on chronic diseases such as healthy eating policies, physical activity policies, and tobacco policies can improve student health behaviours or knowledge of staffs and students.[29][needs update] Encouraging those with chronic conditions to continue with their outpatient (ambulatory) medical care and attend scheduled medical appointments may help improve outcomes and reduce medical costs due to missed appointments.[30] Finding patient-centered alternatives to doctors or consultants scheduling medical appointments has been suggested as a means of improving the number of people with chronic conditions that miss medical appointments, however there is no strong evidence that these approaches make a difference.[30]
Nursing facilities & costing
Nursing can play an important role in assisting patients with chronic diseases achieve longevity and experience wellness.[31] Scholars point out that the current neoliberal era emphasizes self-care, in both affluent and low-income communities.[32] This self-care focus extends to the nursing of patients with chronic diseases, replacing a more holistic role for nursing with an emphasis on patients managing their own health conditions. Critics note that this is challenging if not impossible for patients with chronic disease in low-income communities where health care systems, and economic and social structures do not fully support this practice.[32]
A study in Ethiopia showcases a nursing-heavy approach to the management of chronic disease. Foregrounding the problem of distance from healthcare facility, the study recommends patients increase their request for care. It uses nurses and health officers to fill, in a cost-efficient way, the large unmet need for chronic disease treatment.[33] They led their health centers manned by nurses and health officers; so, there are specific training required for involvement in the programmed must be carried out regularly, to ensure that new staff is educated in administering chronic disease care.[33] The program shows that community-based care and education, primarily driven by nurses and health officers, works.[33] It highlights the importance of nurses following up with individuals in the community, and allowing nurses flexibility in meeting their patients' needs and educating them for self-care in their homes.[citation needed]
Epidemiology globally
The epidemiology of chronic disease is diverse and the epidemiology of some chronic diseases can change in response to new treatments. In the treatment of HIV, the success of anti-retroviral therapies means that many patients will experience this infection as a chronic disease that for many will span several decades of their chronic life.[34]
Some epidemiology of chronic disease can apply to multiple diagnosis. Obesity and body fat distribution for example contribute and are risk factors for many chronic diseases such as diabetes, heart, and kidney disease.[35] Other epidemiological factors, such as social, socioeconomic, and environment do not have a straightforward cause and effect relationship with chronic disease diagnosis. While typically higher socioeconomic status is correlated with lower occurrence of chronic disease, it is not known is there is a direct cause and effect relationship between these two variables.[36]
The epidemiology of communicable chronic diseases such as AIDS is also different from that of noncommunicable chronic disease. While Social factors do play a role in AIDS prevalence, only exposure is truly needed to contract this chronic disease. Communicable chronic diseases are also typically only treatable with medication intervention, rather than lifestyle change as some non-communicable chronic diseases can be treated".[37]
In United States.....
"As of 2003, there are a few programs which aim to gain more knowledge on the epidemiology of chronic disease using data collection. The hope of these programs is to gather epidemiological data on various chronic diseases across the United States and demonstrate how this knowledge can be valuable in addressing chronic disease.[38]
In the United States, as of 2004 nearly one in two Americans (133 million) has at least one chronic medical condition, with most subjects (58%) between the ages of 18 and 64.[13] The number is projected to increase by more than one percent per year by 2030, resulting in an estimated chronically ill population of 171 million.[13] The most common chronic conditions are high blood pressure, arthritis, respiratory diseases like emphysema, and high cholesterol.[citation needed]
Based on data from 2014 Medical Expenditure Panel Survey (MEPS), about 60% of adult Americans were estimated to have one chronic illness, with about 40% having more than one; this rate appears to be mostly unchanged from 2008.[39] MEPS data from 1998 showed 45% of adult Americans had at least one chronic illness, and 21% had more than one.[40]
According to research by the CDC, chronic disease is also especially a concern in the elderly population in America. Chronic diseases like stroke, heart disease, and cancer were among the leading causes of death among Americans aged 65 or older in 2002, accounting for 61% of all deaths among this subset of the population.[41] It is estimated that at least 80% of older Americans are currently living with some form of a chronic condition, with 50% of this population having two or more chronic conditions.[41] The two most common chronic conditions in the elderly are high blood pressure and arthritis, with diabetes, coronary heart disease, and cancer also being reported among the elder population.[42]
In examining the statistics of chronic disease among the living elderly, it is also important to make note of the statistics pertaining to fatalities as a result of chronic disease. Heart disease is the leading cause of death from chronic disease for adults older than 65, followed by cancer, stroke, diabetes, chronic lower respiratory diseases, influenza and pneumonia, and, finally, Alzheimer's disease.[41] Though the rates of chronic disease differ by race for those living with chronic illness, the statistics for leading causes of death among elderly are nearly identical across racial/ethnic groups.[41]
Chronic illnesses cause about 70% of deaths in the US and in 2002 chronic conditions (heart disease, cancers, stroke, chronic respiratory diseases, diabetes, Alzheimer's disease, mental illness and kidney diseases) were 6 of the top ten causes of mortality in the general US population.[43]
Economic impact ---- So high, It's not affordable for all in any country globally for treating properly.
In United States
Chronic diseases are a major factor in the continuous growth of medical care spending.[44] In 2002, the U.S. Department of Health and Human Services stated that the health care for chronic diseases cost the most among all health problems in the U.S.[45] Healthy People 2010 reported that more than 75% of the $2 trillion spent annually in U.S. medical care are due to chronic conditions; spending are even higher in proportion for Medicare beneficiaries (aged 65 years and older).[20] Furthermore, in 2017 it was estimated that 90% of the $3.3 billion spent on healthcare in the United States was due to the treatment of chronic diseases and conditions.[46][47] Spending growth is driven in part by the greater prevalence of chronic illnesses and the longer life expectancy of the population. Also, improvement in treatments has significantly extended the lifespans of patients with chronic diseases but results in additional costs over long period of time. A striking success is the development of combined antiviral therapies that led to remarkable improvement in survival rates and quality of life of HIV-infected patients.
In addition to direct costs in health care, chronic diseases are a significant burden to the economy, through limitations in daily activities, loss in productivity and loss of days of work. A particular concern is the rising rates of overweight and obesity in all segments of the U.S. population.[20] Obesity itself is a medical condition and not a disease, but it constitutes a major risk factor for developing chronic illnesses, such as diabetes, stroke, cardiovascular disease and cancers. Obesity results in significant health care spending and indirect costs, as illustrated by a recent study from the Texas comptroller reporting that obesity alone cost Texas businesses an extra $9.5 billion in 2009, including more than $4 billion for health care, $5 billion for lost productivity and absenteeism, and $321 million for disability.[48]
There have been recent links between social factors and prevalence as well as outcome of chronic conditions.
Specifically, the connection between loneliness and health and chronic condition has recently been highlighted. Some studies have shown that loneliness has detrimental health effects similar to that of smoking and obesity.[49] One study found that feelings of isolation are associated with higher self reporting of health as poor, and feelings of loneliness increased the likelihood of mental health disorders in individuals.[50] The connection between chronic illness and loneliness is established, yet oftentimes ignored in treatment. One study for example found that a greater number of chronic illnesses per individual were associated with feelings of loneliness.[51] Some of the possible reasons for this listed are an inability to maintain independence as well as the chronic illness being a source of stress for the individual. A study of loneliness in adults over age 65 found that low levels of loneliness as well as high levels of familial support were associated with better outcomes of multiple chronic conditions such as hypertension and diabetes.[51] There are some recent movements in the medical sphere to address these connections when treating patients with chronic illness. The biopsychosocial approach for example, developed in 2006 focuses on patients "patient's personality, family, culture, and health dynamics."[52] Physicians are leaning more towards a psychosocial approach to chronic illness to aid the increasing number of individuals diagnosed with these conditions. Despite this movement, there is still criticism that chronic conditions are not being treated appropriately, and there is not enough emphasis on the behavioral aspects of chronic conditions[53] or psychological types of support for patients.[54]
The mental toll of chronic illness is often underestimated in society. Adults with chronic illness that restrict their daily life present with more depression and lower self-esteem than healthy adults and adults with non-restricting chronic illness.[55] The emotional influence of chronic illness also has an effect on the intellectual and educational development of the individual.[56] For example, people living with type 1 diabetes endure a lifetime of monotonous and rigorous health care management usually involving daily blood glucose monitoring, insulin injections, and constant self-care. This type of constant attention that is required by type 1 diabetes and other chronic illness can result in psychological maladjustment. There have been several theories, namely one called diabetes resilience theory, that posit that protective processes buffer the impact of risk factors on the individual's development and functioning.[57]
People with chronic conditions pay more out-of-pocket; a study of the United States found that people spent $2,243 more on average.[58] The financial burden can increase medication non-adherence.[59][60]
In some countries, laws protect patients with chronic conditions from excessive financial responsibility; for example, as of 2008 France limited copayments for those with chronic conditions, and Germany limits cost sharing to 1% of income versus 2% for the general public.[61]
Within the medical-industrial complex, chronic illnesses can impact the relationship between pharmaceutical companies and people with chronic conditions. Life-saving drugs, or life-extending drugs, can be inflated for a profit.[62] There is little regulation on the cost of chronic illness drugs, which suggests that abusing the lack of a drug cap can create a large market for drug revenue.[63] Likewise, certain chronic conditions can last throughout one's lifetime and create pathways for pharmaceutical companies to take advantage of this".[64]
We're for all- ALL are for us for the greater interest of Humanism-Truth-Facts-Friendship-Unity-Participation to a Well-furnished GOAL of Truth from which all shall have ++++;
We're indebted to WIKIPEDIA +WHO for a short while and as 'Guardian QUOTATION' from Global WISER ONE. And have quoted many images, article's, writings etc. by great & humanist writers+++ from global thinkers, Well-wishers, Wiseman, Humanists and Others Living-Nonlivings in favor of HUMANISM to share more answers of Researchers-readers+++++....
To reach the 'GOAL of FULFILNESS' unitedly to alive in the "DESTINATION of TRUTH-FACTS-CHARMEST AMICABLITY" of Natural Joyful POSSIBILITIES+++
BREAST CANCER, TUMOR, Arsenic+Chemical Poisoning, Corona, Heart-Lung diseases, Neurological-Hormonal-Immunal-Infectious diseases with related complexities are possible to cure properly-easily-scientifically-accurately (100%) by our positive medical services only with+++++balance confirming
Medicine-Food control-proper nursing-medicinal massage-Medicinal Yogas- Meditation, Physiotherapy special etc. without side effects & Repeatation as per contract through user-friendly approved ways of CURE++++. please fill our form as below or click:
After confirming contract-letter between you+++. We serve you properly with no Chemo-therapy-radiation therapy -SURGICAL Complexities (Physical-Mental) to CURE+++ upto our Limit to recover your both-health from illness.