We're for all- ALL are for us for the greater interest of Humanism-Truth-Facts-Friendship-Unity-Participation including Physico-Mental Sound Health with Spirituality enrichment through ''TOTAL HEALTH SOLUTION'' to a Well-furnished GOALofTruth alloted for all in real sense ;
From wikipedia & other reliable sources ( Poets, Writers, Thinkers, Researchers, Free Lancers, Philosophers, Theologists, Scientists, Orators, Sociologists and Photographers +Artists-Musicians & etc.) we can learn as follows :
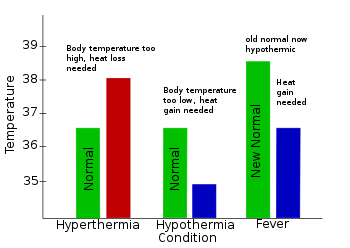

''Fever, also referred to as pyrexia, is defined as having a temperature above the normal range due to an increase in the body's temperature set point.[5][6][12][7] There is not a single agreed-upon upper limit for normal temperature with sources using values between 37.2 and 38.3 °C (99.0 and 100.9 °F) in humans.[1][7][8] The increase in set point triggers increased muscle contractions and causes a feeling of cold or chills.[2] This results in greater heat production and efforts to conserve heat.[3] When the set point temperature returns to normal, a person feels hot, becomes flushed, and may begin to sweat.[3] Rarely a fever may trigger a febrile seizure, with this being more common in young children.[4] Fevers do not typically go higher than 41 to 42 °C (106 to 108 °F).[6]
A fever can be caused by many medical conditions ranging from non-serious to life-threatening.[13] This includes viral, bacterial, and parasitic infections—such as influenza, the common cold, meningitis, urinary tract infections, appendicitis, Lassa, COVID-19, and malaria.[13][14] Non-infectious causes include vasculitis, deep vein thrombosis, connective tissue disease, side effects of medication or vaccination, and cancer.[13][15] It differs from hyperthermia, in that hyperthermia is an increase in body temperature over the temperature set point, due to either too much heat production or not enough heat loss.[1]
Treatment to reduce fever is generally not required.[2][9] Treatment of associated pain and inflammation, however, may be useful and help a person rest.[9] Medications such as ibuprofen or paracetamol (acetaminophen) may help with this as well as lower temperature.[9][10] Children younger than three months require medical attention, as might people with serious medical problems such as a compromised immune system or people with other symptoms.[16] Hyperthermia requires treatment.[2]
Fever is one of the most common medical signs.[2] It is part of about 30% of healthcare visits by children[2] and occurs in up to 75% of adults who are seriously sick.[11] While fever evolved as a defense mechanism, treating a fever does not appear to improve or worsen outcomes.[17][18][19] Fever is often viewed with greater concern by parents and healthcare professionals than is usually deserved, a phenomenon known as fever phobia.
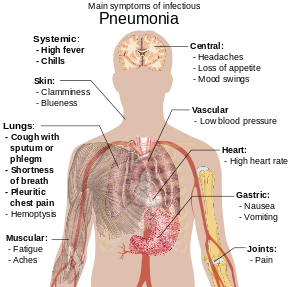
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli.[3][14] Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing.[15] The severity of the condition is variable.[15]
Pneumonia is usually caused by infection with viruses or bacteria, and less commonly by other microorganisms.[a] Identifying the responsible pathogen can be difficult. Diagnosis is often based on symptoms and physical examination.[8] Chest X-rays, blood tests, and culture of the sputum may help confirm the diagnosis.[8] The disease may be classified by where it was acquired, such as community- or hospital-acquired or healthcare-associated pneumonia.[18]
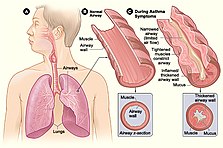
Risk factors for pneumonia include cystic fibrosis, chronic obstructive pulmonary disease (COPD), sickle cell disease, asthma, diabetes, heart failure, a history of smoking, a poor ability to cough (such as following a stroke), and a weak immune system.[5][7]
Vaccines to prevent certain types of pneumonia (such as those caused by Streptococcus pneumoniae bacteria, linked to influenza, or linked to COVID-19) are available.[10] Other methods of prevention include hand washing to prevent infection, not smoking, and social distancing.[10]
Treatment depends on the underlying cause.[19] Pneumonia believed to be due to bacteria is treated with antibiotics.[11] If the pneumonia is severe, the affected person is generally hospitalized.[19] Oxygen therapy may be used if oxygen levels are low.[11]
Each year, pneumonia affects about 450 million people globally (7% of the population) and results in about 4 million deaths.[12][13] With the introduction of antibiotics and vaccines in the 20th century, survival has greatly improved.[12] Nevertheless, pneumonia remains a leading cause of death in developing countries, and also among the very old, the very young, and the chronically ill.[12][20] Pneumonia often shortens the period of suffering among those already close to death and has thus been called "the old man's friend
range for normal temperatures has been found.[8] Central temperatures, such as rectal temperatures, are more accurate than peripheral temperatures.[30] Fever is generally agreed to be present if the elevated temperature[31] is caused by a raised set point and:
- Temperature in the anus (rectum/rectal) is at or over 37.5–38.3 °C (99.5–100.9 °F)[1][8] An ear (tympanic) or forehead (temporal) temperature may also be used.[32][33]
- Temperature in the mouth (oral) is at or over 37.2 °C (99.0 °F) in the morning or over 37.7 °C (99.9 °F) in the afternoon[7][34]
- Temperature under the arm (axillary) is usually about 0.6 °C (1.1 °F) below core body temperature.[35]
In adults, the normal range of oral temperatures in healthy individuals is 35.7–37.7 °C (96.3–99.9 °F) among men and 33.2–38.1 °C (91.8–100.6 °F) among women, while when taken rectally it is 36.7–37.5 °C (98.1–99.5 °F) among men and 36.8–37.1 °C (98.2–98.8 °F) among women, and for ear measurement it is 35.5–37.5 °C (95.9–99.5 °F) among men and 35.7–37.5 °C (96.3–99.5 °F) among women.[36]
Normal body temperatures vary depending on many factors, including age, sex, time of day, ambient temperature, activity level, and more.[37][38] Normal daily temperature variation has been described as 0.5 °C (0.9 °F).[7]: 4012 A raised temperature is not always a fever.[37] For example, the temperature rises in healthy people when they exercise, but this is not considered a fever, as the set point is normal.[37] On the other hand, a "normal" temperature may be a fever, if it is unusually high for that person; for example, medically frail elderly people have a decreased ability to generate body heat, so a "normal" temperature of 37.3 °C (99.1 °F) may represent a clinically significant fever.[37][39]
Hyperthermia[edit]
Hyperthermia is an elevation of body temperature over the temperature set point, due to either too much heat production or not enough heat loss.[1][7] Hyperthermia is thus not considered fever.[7]: 103 [40] Hyperthermia is not to be confused with hyperpyrexia (which is a very high fever).[7]: 102
Clinically, it is important to distinguish between fever and hyperthermia as hyperthermia may quickly lead to death and does not respond to antipyretic medications. The distinction may however be difficult to make in an emergency setting, and is often established by identifying possible causes.[7]: 103
Types[edit]
Various patterns of measured patient temperatures have been observed, some of which may be indicative of a particular medical diagnosis:
- Continuous fever, where temperature remains above normal and does not fluctuate more than 1 °C in 24 hours[41] (e.g. in bacterial pneumonia, typhoid, infective endocarditis, tuberculosis, or typhus.[42][43]
- Intermittent fever is present only for a certain period, later cycling back to normal (e.g., in malaria, leishmaniasis, pyemia, sepsis,[44] or African trypanosomiasis.[45]
- Remittent fever, where the temperature remains above normal throughout the day and fluctuates more than 1 °C in 24 hours (e.g., in infective endocarditis or brucellosis).[46]
- Pel–Ebstein fever is a cyclic fever that is rarely seen in patients with Hodgkin's lymphoma.
- Undulant fever, seen in brucellosis.
- Typhoid fever is a continuous fever showing a characteristic step-ladder pattern, a step-wise increase in temperature with a high plateau.[47]
Among the types of intermittent fever are ones specific to cases of malaria caused by different pathogens. These are:[48][49]
- Quotidian fever, with a 24-hour periodicity, typical of malaria caused by Plasmodium knowlesi (P. knowlesi);[50][51]
- Tertian fever, with a 48-hour periodicity, typical of later course malaria caused by P. falciparum, P. vivax, or P. ovale;[48]
- Quartan fever, with a 72-hour periodicity, typical of later course malaria caused by P. malariae.[48]
In addition, there is disagreement regarding whether a specific fever pattern is associated with Hodgkin's lymphoma—the Pel–Ebstein fever, with patients argued to present high temperature for one week, followed by low for the next week, and so on, where the generality of this pattern is debated.[52][53]
Persistent fever that cannot be explained after repeated routine clinical inquiries is called fever of unknown origin.[7][54] A neutropenic fever, also called febrile neutropenia, is a fever in the absence of normal immune system function.[55] Because of the lack of infection-fighting neutrophils, a bacterial infection can spread rapidly; this fever is, therefore, usually considered to require urgent medical attention.[56] This kind of fever is more commonly seen in people receiving immune-suppressing chemotherapy than in apparently healthy people.[55][57]
Hyperpyrexia[edit]--- Hyperpyrexia is an extreme elevation of body temperature which, depending upon the source, is classified as a core body temperature greater than or equal to 40 or 41 °C (104 or 106 °F); the range of hyperpyrexias includes cases considered severe (≥ 40 °C) and extreme (≥ 42 °C).[7][58][59] It differs from hyperthermia in that one's thermoregulatory system's set point for body temperature is set above normal, then heat is generated to achieve it. In contrast, hyperthermia involves body temperature rising above its set point due to outside factors.[7][60] The high temperatures of hyperpyrexia are considered medical emergencies, as they may indicate a serious underlying condition or lead to severe morbidity (including permanent brain damage), or to death.[61] A common cause of hyperpyrexia is an intracranial hemorrhage.[7] Other causes in emergency room settings include sepsis, Kawasaki syndrome,[62] neuroleptic malignant syndrome, drug overdose, serotonin syndrome, and thyroid storm.[61]
Differential diagnosis[edit] Fever is a common symptom of many medical conditions:
- Infectious disease, e.g., COVID-19,[14] dengue, Ebola, gastroenteritis, HIV, influenza, Lyme disease, rocky mountain spotted fever, secondary syphilis, malaria, mononucleosis, as well as infections of the skin, e.g., abscesses and boils.[63][64][65][66][67][68]
- Immunological diseases, e.g., relapsing polychondritis,[69] autoimmune hepatitis, granulomatosis with polyangiitis, Horton disease, inflammatory bowel diseases, Kawasaki disease, lupus erythematosus, sarcoidosis, and Still's disease;[citation needed]
- Tissue destruction, as a result of cerebral bleeding, crush syndrome, hemolysis, infarction, rhabdomyolysis, surgery, etc.;[70][71]
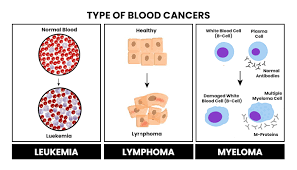
- Cancers, particularly blood cancers such as leukemia and lymphomas;[72]
- Metabolic disorders, e.g., gout, and porphyria;[73] and[74]
- Inherited metabolic disorder, e.g., Fabry disease.[7]
Adult and pediatric manifestations for the same disease may differ; for instance, in COVID-19, one metastudy describes 92.8% of adults versus 43.9% of children presenting with fever.[14]
In addition, fever can result from a reaction to an incompatible blood product.[75]
Teething is not a cause of fever.
Pneumonia People with infectious pneumonia often have a productive cough, fever accompanied by shaking chills, shortness of breath, sharp or stabbing chest pain during deep breaths, and an increased rate of breathing.[9] In elderly people, confusion may be the most prominent sign.[9]
The typical signs and symptoms in children under five are fever, cough, and fast or difficult breathing.[23] Fever is not very specific, as it occurs in many other common illnesses and may be absent in those with severe disease, malnutrition or in the elderly. In addition, a cough is frequently absent in children less than 2 months old.[23] More severe signs and symptoms in children may include blue-tinged skin, unwillingness to drink, convulsions, ongoing vomiting, extremes of temperature, or a decreased level of consciousness.[23][24]
Bacterial and viral cases of pneumonia usually result in similar symptoms.[25] Some causes are associated with classic, but non-specific, clinical characteristics. Pneumonia caused by Legionella may occur with abdominal pain, diarrhea, or confusion.[26] Pneumonia caused by Streptococcus pneumoniae is associated with rusty colored sputum.[27] Pneumonia caused by Klebsiella may have bloody sputum often described as "currant jelly".[22] Bloody sputum (known as hemoptysis) may also occur with tuberculosis, Gram-negative pneumonia, lung abscesses and more commonly acute bronchitis.[24] Pneumonia caused by Mycoplasma pneumoniae may occur in association with swelling of the lymph nodes in the neck, joint pain, or a middle ear infection.[24] Viral pneumonia presents more commonly with wheezing than bacterial pneumonia.[25] Pneumonia was historically divided into "typical" and "atypical" based on the belief that the presentation predicted the underlying cause.[28] However, evidence has not supported this distinction, therefore it is no longer emphasized.[28]
 The bacterium Streptococcus pneumoniae, a common cause of pneumonia, imaged by an electron microscope
The bacterium Streptococcus pneumoniae, a common cause of pneumonia, imaged by an electron microscope
Pneumonia is due to infections caused primarily by bacteria or viruses and less commonly by fungi and parasites. Although more than 100 strains of infectious agents have been identified, only a few are responsible for the majority of cases. Mixed infections with both viruses and bacteria may occur in roughly 45% of infections in children and 15% of infections in adults.[12] A causative agent may not be isolated in about half of cases despite careful testing.[21] In an active population-based surveillance for community-acquired pneumonia requiring hospitalization in five hospitals in Chicago and Nashville from January 2010 through June 2012, 2259 patients were identified who had radiographic evidence of pneumonia and specimens that could be tested for the responsible pathogen.[29] Most patients (62%) had no detectable pathogens in their sample, and unexpectedly, respiratory viruses were detected more frequently than bacteria.[29] Specifically, 23% had one or more viruses, 11% had one or more bacteria, 3% had both bacterial and viral pathogens, and 1% had a fungal or mycobacterial infection. "The most common pathogens were human rhinovirus (in 9% of patients), influenza virus (in 6%), and Streptococcus pneumoniae (in 5%)."[29]
The term pneumonia is sometimes more broadly applied to any condition resulting in inflammation of the lungs (caused for example by autoimmune diseases, chemical burns or drug reactions); however, this inflammation is more accurately referred to as pneumonitis.[16][17]
Factors that predispose to pneumonia include smoking, immunodeficiency, alcoholism, chronic obstructive pulmonary disease, sickle cell disease (SCD), asthma, chronic kidney disease, liver disease, and biological aging.[24][30][7] Additional risks in children include not being breastfed, exposure to cigarette smoke and other air pollution, malnutrition, and poverty.[31] The use of acid-suppressing medications – such as proton-pump inhibitors or H2 blockers – is associated with an increased risk of pneumonia.[32] Approximately 10% of people who require mechanical ventilation develop ventilator-associated pneumonia,[33] and people with a gastric feeding tube have an increased risk of developing aspiration pneumonia.[34] For people with certain variants of the FER gene, the risk of death is reduced in sepsis caused by pneumonia. However, for those with TLR6 variants, the risk of getting Legionnaires' disease is increased.[35]
Bacteria: Bacterial pneumonia Cavitating pneumonia due to MRSA as seen on a CT scan
Cavitating pneumonia due to MRSA as seen on a CT scan
Bacteria are the most common cause of community-acquired pneumonia (CAP), with Streptococcus pneumoniae isolated in nearly 50% of cases.[36][37] Other commonly isolated bacteria include Haemophilus influenzae in 20%, Chlamydophila pneumoniae in 13%, and Mycoplasma pneumoniae in 3% of cases;[36] Staphylococcus aureus; Moraxella catarrhalis; and Legionella pneumophila.[21] A number of drug-resistant versions of the above infections are becoming more common, including drug-resistant Streptococcus pneumoniae (DRSP) and methicillin-resistant Staphylococcus aureus (MRSA).[24]
The spreading of organisms is facilitated by certain risk factors.[21] Alcoholism is associated with Streptococcus pneumoniae, anaerobic organisms, and Mycobacterium tuberculosis; smoking facilitates the effects of Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and Legionella pneumophila. Exposure to birds is associated with Chlamydia psittaci; farm animals with Coxiella burnetti; aspiration of stomach contents with anaerobic organisms; and cystic fibrosis with Pseudomonas aeruginosa and Staphylococcus aureus.[21] Streptococcus pneumoniae is more common in the winter,[21] and it should be suspected in persons aspirating a large number of anaerobic organisms.[24]
Noninfectious: Idiopathic interstitial pneumonia
Idiopathic interstitial pneumonia or noninfectious pneumonia[46] is a class of diffuse lung diseases. They include diffuse alveolar damage, organizing pneumonia, nonspecific interstitial pneumonia, lymphocytic interstitial pneumonia, desquamative interstitial pneumonia, respiratory bronchiolitis interstitial lung disease, and usual interstitial pneumonia.[47] Lipoid pneumonia is another rare cause due to lipids entering the lung.[48] These lipids can either be inhaled or spread to the lungs from elsewhere in the body.[48]
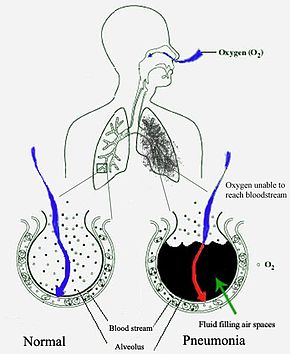
 Pneumonia fills the lung's alveoli with fluid, hindering oxygenation. The alveolus on the left is normal, whereas the one on the right is full of fluid from pneumonia.
Pneumonia fills the lung's alveoli with fluid, hindering oxygenation. The alveolus on the left is normal, whereas the one on the right is full of fluid from pneumonia.
Pneumonia frequently starts as an upper respiratory tract infection that moves into the lower respiratory tract.[49] It is a type of pneumonitis (lung inflammation).[50] The normal flora of the upper airway give protection by competing with pathogens for nutrients. In the lower airways, reflexes of the glottis, actions of complement proteins and immunoglobulins are important for protection. Microaspiration of contaminated secretions can infect the lower airways and cause pneumonia. The progress of pneumonia is determined by the virulence of the organism; the amount of organism required to start an infection; and the body's immune response against the infection.[35]
Most bacteria enter the lungs via small aspirations of organisms residing in the throat or nose.[24] Half of normal people have these small aspirations during sleep.[28] While the throat always contains bacteria, potentially infectious ones reside there only at certain times and under certain conditions.[28] A minority of types of bacteria such as Mycobacterium tuberculosis and Legionella pneumophila reach the lungs via contaminated airborne droplets.[24] Bacteria can also spread via the blood.[25] Once in the lungs, bacteria may invade the spaces between cells and between alveoli, where the macrophages and neutrophils (defensive white blood cells) attempt to inactivate the bacteria.[51] The neutrophils also release cytokines, causing a general activation of the immune system.[52] This leads to the fever, chills, and fatigue common in bacterial pneumonia.[52] The neutrophils, bacteria, and fluid from surrounding blood vessels fill the alveoli, resulting in the consolidation seen on chest X-ray.[53]
Viruses may reach the lung by a number of different routes. Respiratory syncytial virus is typically contracted when people touch contaminated objects and then touch their eyes or nose.[38] Other viral infections occur when contaminated airborne droplets are inhaled through the nose or mouth.[24] Once in the upper airway, the viruses may make their way into the lungs, where they invade the cells lining the airways, alveoli, or lung parenchyma.[38] Some viruses such as measles and herpes simplex may reach the lungs via the blood.[54] The invasion of the lungs may lead to varying degrees of cell death.[38] When the immune system responds to the infection, even more lung damage may occur.[38] Primarily white blood cells, mainly mononuclear cells, generate the inflammation.[54] As well as damaging the lungs, many viruses simultaneously affect other organs and thus disrupt other body functions. Viruses also make the body more susceptible to bacterial infections; in this way, bacterial pneumonia can occur at the same time as viral pneumonia.[39]
Pneumonia is typically diagnosed based on a combination of physical signs and often a chest X-ray.[55] In adults with normal vital signs and a normal lung examination, the diagnosis is unlikely.[56] However, the underlying cause can be difficult to confirm, as there is no definitive test able to distinguish between bacterial and non-bacterial cause.[12][55] The overall impression of a physician appears to be at least as good as decision rules for making or excluding the diagnosis.[57]
The World Health Organization has defined pneumonia in children clinically based on either a cough or difficulty breathing and a rapid respiratory rate, chest indrawing, or a decreased level of consciousness.[58] A rapid respiratory rate is defined as greater than 60 breaths per minute in children under 2 months old, greater than 50 breaths per minute in children 2 months to 1 year old, or greater than 40 breaths per minute in children 1 to 5 years old.[58]
In children, low oxygen levels and lower chest indrawing are more sensitive than hearing chest crackles with a stethoscope or increased respiratory rate.[59] Grunting and nasal flaring may be other useful signs in children less than five years old.[60]
Lack of wheezing is an indicator of Mycoplasma pneumoniae in children with pneumonia, but as an indicator it is not accurate enough to decide whether or not macrolide treatment should be used.[61] The presence of chest pain in children with pneumonia doubles the probability of Mycoplasma pneumoniae.[61]
In general, in adults, investigations are not needed in mild cases.[62] There is a very low risk of pneumonia if all vital signs and auscultation are normal.[63] C-reactive protein (CRP) may help support the diagnosis.[64] For those with CRP less than 20 mg/L without convincing evidence of pneumonia, antibiotics are not recommended.[35]
Procalcitonin may help determine the cause and support decisions about who should receive antibiotics.[65] Antibiotics are encouraged if the procalcitonin level reaches 0.25 μg/L, strongly encouraged if it reaches 0.5 μg/L, and strongly discouraged if the level is below 0.10 μg/L.[35] In people requiring hospitalization, pulse oximetry, chest radiography and blood tests – including a complete blood count, serum electrolytes, C-reactive protein level, and possibly liver function tests – are recommended.[62]
The diagnosis of influenza-like illness can be made based on the signs and symptoms; however, confirmation of an influenza infection requires testing.[66] Thus, treatment is frequently based on the presence of influenza in the community or a rapid influenza test.[66]
Physical examination may sometimes reveal low blood pressure, high heart rate, or low oxygen saturation.[24] The respiratory rate may be faster than normal, and this may occur a day or two before other signs.[24][28] Examination of the chest may be normal, but it may show decreased expansion on the affected side. Harsh breath sounds from the larger airways that are transmitted through the inflamed lung are termed bronchial breathing and are heard on auscultation with a stethoscope.[24] Crackles (rales) may be heard over the affected area during inspiration.[24] Percussion may be dulled over the affected lung, and increased, rather than decreased, vocal resonance distinguishes pneumonia from a pleural effusion.[9]
A chest radiograph is frequently used in diagnosis.[23] In people with mild disease, imaging is needed only in those with potential complications, those not having improved with treatment, or those in which the cause is uncertain.[23][62] If a person is sufficiently sick to require hospitalization, a chest radiograph is recommended.[62] Findings do not always match the severity of disease and do not reliably separate between bacterial and viral infection.[23]
X-ray presentations of pneumonia may be classified as lobar pneumonia, bronchopneumonia, lobular pneumonia, and interstitial pneumonia.[67] Bacterial, community-acquired pneumonia classically show lung consolidation of one lung segmental lobe, which is known as lobar pneumonia.[36] However, findings may vary, and other patterns are common in other types of pneumonia.[36] Aspiration pneumonia may present with bilateral opacities primarily in the bases of the lungs and on the right side.[36] Radiographs of viral pneumonia may appear normal, appear hyper-inflated, have bilateral patchy areas, or present similar to bacterial pneumonia with lobar consolidation.[36] Radiologic findings may not be present in the early stages of the disease, especially in the presence of dehydration, or may be difficult to interpret in the obese or those with a history of lung disease.[24] Complications such as pleural effusion may also be found on chest radiographs. Laterolateral chest radiographs can increase the diagnostic accuracy of lung consolidation and pleural effusion.[35]
A CT scan can give additional information in indeterminate cases.[36] CT scans can also provide more details in those with an unclear chest radiograph (for example occult pneumonia in chronic obstructive pulmonary disease) and can exclude pulmonary embolism and fungal pneumonia and detect lung abscess in those who are not responding to treatments.[35] However, CT scans are more expensive, have a higher dose of radiation, and cannot be done at bedside.[35]
Lung ultrasound may also be useful in helping to make the diagnosis.[68] Ultrasound is radiation free and can be done at bedside. However, ultrasound requires specific skills to operate the machine and interpret the findings.[35] It may be more accurate than chest X-ray.[69]
- ---
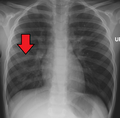 Right middle lobe pneumonia in a child as seen on plain X-ray
Right middle lobe pneumonia in a child as seen on plain X-ray
In people managed in the community, determining the causative agent is not cost-effective and typically does not alter management.[23] For people who do not respond to treatment, sputum culture should be considered, and culture for Mycobacterium tuberculosis should be carried out in persons with a chronic productive cough.[62] Microbiological evaluation is also indicated in severe pneumonia, alcoholism, asplenia, immunosuppression, HIV infection, and those being empirically treated for MRSA of pseudomonas.[35][71] Although positive blood culture and pleural fluid culture definitively establish the diagnosis of the type of micro-organism involved, a positive sputum culture has to be interpreted with care for the possibility of colonisation of respiratory tract.[35] Testing for other specific organisms may be recommended during outbreaks, for public health reasons.[62] In those hospitalized for severe disease, both sputum and blood cultures are recommended,[62] as well as testing the urine for antigens to Legionella and Streptococcus.[72] Viral infections, can be confirmed via detection of either the virus or its antigens with culture or polymerase chain reaction (PCR), among other techniques.[12] Mycoplasma, Legionella, Streptococcus, and Chlamydia can also be detected using PCR techniques on bronchoalveolar lavage and nasopharyngeal swab.[35] The causative agent is determined in only 15% of cases with routine microbiological tests''.[9]
We're for all- ALL are for us for the greater interest of Humanism-Truth-Facts-Friendship-Unity-Participation to a Well-furnished GOAL of Truth from which all shall have ++++;
We're indebted to WIKIPEDIA +WHO for a short while and as 'Guardian QUOTATION' from Global WISER ONE. And have quoted many images, article's, writings etc. by great & humanist writers+++ from global thinkers, Well-wishers, Wiseman, Humanists and Others Living-Nonlivings in favor of HUMANISM to share more answers of Researchers-readers+++++....
To reach the 'GOAL of FULFILNESS' unitedly to alive in the "DESTINATION of TRUTH-FACTS-CHARMEST AMICABLITY" of Natural Joyful POSSIBILITIES+++
BREAST CANCER, TUMOR, Arsenic+Chemical Poisoning, Corona, Heart-Lung diseases, Neurological-Hormonal-Immunal-Infectious diseases with related complexities are possible to cure properly-easily-scientifically-accurately (100%) by our positive medical services only with+++++balance confirming
Medicine-Food control-proper nursing-medicinal massage-Medicinal Yogas- Meditation, Physiotherapy special etc. without side effects & Repeatation as per contract through user-friendly approved ways of CURE++++. please fill our form as below or click:
After confirming contract-letter between you+++. We serve you properly with no Chemo-therapy-radiation therapy -SURGICAL Complexities (Physical-Mental) to CURE+++ upto our Limit to recover your both-health from illness.