We're for all- ALL are for us for the greater interest of Humanism-Truth-Facts-Friendship-Unity-Participation including Physico-Mental Sound Health with Spirituality, enrichment through ''TOTAL HEALTH SOLUTION'' to a Well-furnished GOALofTruth alloted for all in real sense ;
From wikipedia & other reliable sources ( Poets, Writers, Thinkers, Researchers, Free Lancers, Philosophers, Theologists, Scientists, Orators, Sociologists and Photographers +Artists-Musicians & etc.) we can learn as follows :
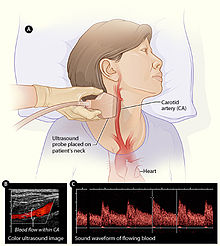

''Pulmonary edema: Lung ultrasound has been shown to be very sensitive for the detection of pulmonary edema. It allows for improvement in diagnosis and management of critically ill patients, particularly when used in combination with echocardiography. The sonographic feature that is present in pulmonary edema is multiple B-lines. B-lines can occur in a healthy lung; however, the presence of 3 or more in the anterior or lateral lung regions is always abnormal. In pulmonary edema, B-lines indicate an increase in the amount of water contained in the lungs outside of the pulmonary vasculature. B-lines can also be present in a number of other conditions including pneumonia, pulmonary contusion, and lung infarction.[30] Additionally, it is important to note that there are multiple types of interactions between the pleural surface and the ultrasound wave that can generate artifacts with some similarity to B-lines but which do not have pathologic significance.[31]

- Pneumothorax: In clinical settings when pneumothorax is suspected, lung ultrasound can aid in diagnosis.[32] In pneumothorax, air is present between the two layers of the pleura and lung sliding on ultrasound is therefore absent. The negative predictive value for lung sliding on ultrasound is reported as 99.2–100% - briefly, if lung sliding is present, a pneumothorax is effectively ruled out.[29] The absence of lung sliding, however, is not necessarily specific for pneumothorax as there are other conditions that also cause this finding including acute respiratory distress syndrome, lung consolidations, pleural adhesions, and pulmonary fibrosis.[29]
- Pleural effusion: Lung ultrasound is a cost-effective, safe, and non-invasive imaging method that can aid in the prompt visualization and diagnosis of pleural effusions. Effusions can be diagnosed by a combination of physical exam, percussion, and auscultation of the chest. However, these exam techniques can be complicated by a variety of factors including the presence of mechanical ventilation, obesity, or patient positioning, all of which reduce the sensitivity of the physical exam. Consequently, lung ultrasound can be an additional tool to augment plain chest Xray and chest CT.[33] Pleural effusions on ultrasound appear as structural images within the thorax rather than an artifact. They will typically have four distinct borders including the pleural line, two rib shadows, and a deep border.[28] In critically ill patients with pleural effusion, ultrasound may guide procedures including needle insertion, thoracentesis, and chest-tube insertion.[33]
- Lung cancer staging: In pulmonology, endobronchial ultrasound (EBUS) probes are applied to standard flexible endoscopic probes and used by pulmonologists to allow for direct visualization of endobronchial lesions and lymph nodes prior to transbronchial needle aspiration. Among its many uses, EBUS aids in lung cancer staging by allowing for lymph node sampling without the need for major surgery.[34]
- COVID-19: Lung ultrasound has proved useful in the diagnosis of COVID-19 especially in cases where other investigations are not available.[35][36][37]
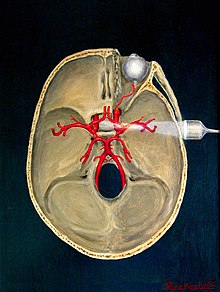
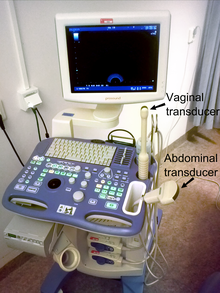 Ultrasound is routinely used in urology to determine the amount of fluid retained in a patient's bladder. In a pelvic sonogram, images include the uterus and ovaries or urinary bladder in females. In males, a sonogram will provide information about the bladder, prostate, or testicles (for example to urgently distinguish epididymitis from testicular torsion). In young males, it is used to distinguish more benign testicular masses (varicocele or hydrocele) from testicular cancer, which is curable but must be treated to preserve health and fertility. There are two methods of performing pelvic sonography – externally or internally. The internal pelvic sonogram is performed either transvaginally (in a woman) or transrectally (in a man). Sonographic imaging of the pelvic floor can produce important diagnostic information regarding the precise relationship of abnormal structures with other pelvic organs and it represents a useful hint to treat patients with symptoms related to pelvic prolapse, double incontinence and obstructed defecation.[citation needed] It is also used to diagnose and, at higher frequencies, to treat (break up) kidney stones or kidney crystals (nephrolithiasis).[38]
Ultrasound is routinely used in urology to determine the amount of fluid retained in a patient's bladder. In a pelvic sonogram, images include the uterus and ovaries or urinary bladder in females. In males, a sonogram will provide information about the bladder, prostate, or testicles (for example to urgently distinguish epididymitis from testicular torsion). In young males, it is used to distinguish more benign testicular masses (varicocele or hydrocele) from testicular cancer, which is curable but must be treated to preserve health and fertility. There are two methods of performing pelvic sonography – externally or internally. The internal pelvic sonogram is performed either transvaginally (in a woman) or transrectally (in a man). Sonographic imaging of the pelvic floor can produce important diagnostic information regarding the precise relationship of abnormal structures with other pelvic organs and it represents a useful hint to treat patients with symptoms related to pelvic prolapse, double incontinence and obstructed defecation.[citation needed] It is also used to diagnose and, at higher frequencies, to treat (break up) kidney stones or kidney crystals (nephrolithiasis).[38]
Scrotal ultrasonography is used in the evaluation of testicular pain, and can help identify solid masses.[39]
Ultrasound is an excellent method for the study of the penis, such as indicated in trauma, priapism, erectile dysfunction or suspected Peyronie's disease.[40]
Musculoskeletal ultrasound is used to examine tendons, muscles, nerves, ligaments, soft tissue masses, and bone surfaces.[41] It is helpful in diagnosing ligament sprains, muscles strains and joint pathology. It is an alternative or supplement to x-ray imaging in detecting fractures of the wrist, elbow and shoulder for patients up to 12 years[42] (Fracture sonography).
Quantitative ultrasound is an adjunct musculoskeletal test for myopathic disease in children;[43][44] estimates of lean body mass in adults;[45] proxy measures of muscle quality (i.e., tissue composition)[46] in older adults with sarcopenia[47][48]
Ultrasound can also be used for needle guidance in muscle or joint injections, as in ultrasound-guided hip joint injection.
In nephrology, ultrasonography of the kidneys is essential in the diagnosis and management of kidney-related diseases. The kidneys are easily examined, and most pathological changes are distinguishable with ultrasound. It is an accessible, versatile, relatively economic, and fast aid for decision-making in patients with renal symptoms and for guidance in renal intervention.[49] Using B-mode imaging, assessment of renal anatomy is easily performed, and US is often used as image guidance for renal interventions. Furthermore, novel applications in renal US have been introduced with contrast-enhanced ultrasound (CEUS), elastography and fusion imaging. However, renal US has certain limitations, and other modalities, such as CT (CECT) and MRI, should be considered for supplementary imaging in assessing renal disease.[49]
--Intravenous access, for the collection of blood samples to assist in diagnosis or laboratory investigation including blood culture, or for administration of intravenous fluids for fluid maintenance of replacement or blood transfusion in sicker patients, is a common medical procedure. The need for intravenous access occurs in the outpatient laboratory, in the inpatient hospital units, and most critically in the Emergency Room and Intensive Care Unit. In many situations, intravenous access may be required repeatedly or over a significant time period. In these latter circumstances, a needle with an overlying catheter is introduced into the vein and the catheter is then inserted securely into the vein while the needle is withdrawn. The chosen veins are most frequently selected from the arm, but in challenging situations, a deeper vein from the neck (external jugular vein) or upper arm (subclavian vein) may need to be used. There are many reasons why the selection of a suitable vein may be problematic. These include, but are not limited to, obesity, previous injury to veins from inflammatory reaction to previous 'blood draws', previous injury to veins from recreational drug use.[citation needed]
In these challenging situations, the insertion of a catheter into a vein has been greatly assisted by the use of ultrasound. The ultrasound unit may be 'cart-based' or 'handheld' using a linear transducer with a frequency of 10 to 15 megahertz. In most circumstances, choice of vein will be limited by the requirement that the vein is within 1.5 cms. from the skin surface. The transducer may be placed longitudinally or transversely over the chosen vein. Ultrasound training for intravenous cannulation is offered in most ultrasound training programs.[citation needed]
- A-mode: A-mode (amplitude mode) is the simplest. A single transducer scans a line through the body with the echoes plotted on screen as a function of depth. Therapeutic ultrasound aimed at a specific tumor or calculus is A-mode, to allow for pinpoint accurate focus of the destructive wave energy.[8]
- B-mode or 2D mode: In B-mode (brightness mode), a linear array of transducers simultaneously scans a plane through the body that can be viewed as a two-dimensional image on screen. More commonly known as 2D mode now.
-
- B-flow is a mode that digitally highlights moving reflectors (mainly red blood cells) while suppressing the signals from the surrounding stationary tissue. It can visualize flowing blood and surrounding stationary tissues simultaneously.[9] It is thus an alternative or complement to Doppler ultrasonography in visualizing blood flow.[10]
- C-mode: A C-mode image is formed in a plane normal to a B-mode image. A gate that selects data from a specific depth from an A-mode line is used; then the transducer is moved in the 2D plane to sample the entire region at this fixed depth. When the transducer traverses the area in a spiral, an area of 100 cm2 can be scanned in around 10 seconds.[7]
- M-mode: In M-mode (motion mode), pulses are emitted in quick succession – each time, either an A-mode or B-mode image is taken. Over time, this is analogous to recording a video in ultrasound. As the organ boundaries that produce reflections move relative to the probe, this can be used to determine the velocity of specific organ structures.
- Doppler mode: This mode makes use of the Doppler effect in measuring and visualizing blood flow
- Color Doppler: Velocity information is presented as a color-coded overlay on top of a B-mode image
- Continuous wave (CW) Doppler: Doppler information is sampled along a line through the body, and all velocities detected at each time point are presented (on a time line)
- Pulsed wave (PW) Doppler: Doppler information is sampled from only a small sample volume (defined in 2D image), and presented on a timeline
- Duplex: The term refers to the fact that 2 modes of ultrasounds are used simultaneously, these are generally simultaneous presentation of 2D (B-mode) and PW Doppler/Color doppler information.
- Triplex: When 2D image (B-mode) and color doppler are combined with Spectral doppler it becomes a Triplex Ultrasound. In the triplex image putting a cursor on any point gives the spectral reading of the point below the image.
- Pulse inversion mode: Two successive pulses with opposite sign are emitted and then subtracted from each other. This implies that any linearly responding constituent will disappear while gases with non-linear compressibility stand out. Pulse inversion may also be used in a similar manner as in Harmonic mode; see below:
- Harmonic mode: A transducer emits fundamental ultrasound pulses into the body and a central, narrow beam of harmonic overtone is reflected back after passing through the bodily tissues. When the harmonic mode is turned on, only this narrow beam of pulses is detected. The fundamental ultrasound pulses and scattered pulses are removed. Thus, lateral and contrast resolutions are improved with this mode''.[11]
Pathology---
''Surgical pathology is one of the primary areas of practice for most anatomical pathologists. Surgical pathology involves the gross and microscopic examination of surgical specimens, as well as biopsies submitted by surgeons and non-surgeons such as general internists, medical subspecialists, dermatologists, and interventional radiologists. Often an excised tissue sample is the best and most definitive evidence of disease (or lack thereof) in cases where tissue is surgically removed from a patient. These determinations are usually accomplished by a combination of gross (i.e., macroscopic) and histologic (i.e., microscopic) examination of the tissue, and may involve evaluations of molecular properties of the tissue by immunohistochemistry or other laboratory tests.[citation needed]

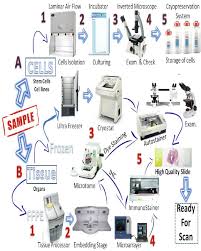
There are two major types of specimens submitted for surgical pathology analysis: biopsies and surgical resections. A biopsy is a small piece of tissue removed primarily for surgical pathology analysis, most often in order to render a definitive diagnosis. Types of biopsies include core biopsies, which are obtained through the use of large-bore needles, sometimes under the guidance of radiological techniques such as ultrasound, CT scan, or magnetic resonance imaging. Incisional biopsies are obtained through diagnostic surgical procedures that remove part of a suspicious lesion, whereas excisional biopsies remove the entire lesion, and are similar to therapeutic surgical resections. Excisional biopsies of skin lesions and gastrointestinal polyps are very common. The pathologist's interpretation of a biopsy is critical to establishing the diagnosis of a benign or malignant tumor, and can differentiate between different types and grades of cancer, as well as determining the activity of specific molecular pathways in the tumor. Surgical resection specimens are obtained by the therapeutic surgical removal of an entire diseased area or organ (and occasionally multiple organs). These procedures are often intended as definitive surgical treatment of a disease in which the diagnosis is already known or strongly suspected, but pathological analysis of these specimens remains important in confirming the previous diagnosis''
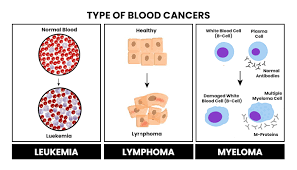
Hematopathology is the study of diseases of blood cells (including constituents such as white blood cells, red blood cells, and platelets) and the tissues, and organs comprising the hematopoietic system. The term hematopoietic system refers to tissues and organs that produce and/or primarily host hematopoietic cells and includes bone marrow, the lymph nodes, thymus, spleen, and other lymphoid tissues. In the United States, hematopathology is a board certified subspecialty (licensed under the American Board of Pathology) practiced by those physicians who have completed a general pathology residency (anatomic, clinical, or combined) and an additional year of fellowship training in hematology. The hematopathologist reviews biopsies of lymph nodes, bone marrows and other tissues involved by an infiltrate of cells of the hematopoietic system. In addition, the hematopathologist may be in charge of flow cytometric and/or molecular hematopathology studies.[citation needed
Molecular pathology is focused upon the study and diagnosis of disease through the examination of molecules within organs, tissues or bodily fluids.[17] Molecular pathology is multidisciplinary by nature and shares some aspects of practice with both anatomic pathology and clinical pathology, molecular biology, biochemistry, proteomics and genetics. It is often applied in a context that is as much scientific as directly medical and encompasses the development of molecular and genetic approaches to the diagnosis and classification of human diseases, the design and validation of predictive biomarkers for treatment response and disease progression, and the susceptibility of individuals of different genetic constitution to particular disorders. The crossover between molecular pathology and epidemiology is represented by a related field "molecular pathological epidemiology".[18] Molecular pathology is commonly used in diagnosis of cancer and infectious diseases. Molecular Pathology is primarily used to detect cancers such as melanoma, brainstem glioma, brain tumors as well as many other types of cancer and infectious diseases.[19] Techniques are numerous but include quantitative polymerase chain reaction (qPCR), multiplex PCR, DNA microarray, in situ hybridization, DNA sequencing, antibody-based immunofluorescence tissue assays, molecular profiling of pathogens, and analysis of bacterial genes for antimicrobial resistance.[20] Techniques used are based on analyzing samples of DNA and RNA. Pathology is widely used for gene therapy and disease diagnosis.[21]
Oral and maxillofacial pathology[edit] Many conditions, such as this case of geographic tongue, can be diagnosed partly on gross examination, but may be confirmed with tissue pathology.
Many conditions, such as this case of geographic tongue, can be diagnosed partly on gross examination, but may be confirmed with tissue pathology.
Oral and Maxillofacial Pathology is one of nine dental specialties recognized by the American Dental Association, and is sometimes considered a specialty of both dentistry and pathology.[22] Oral Pathologists must complete three years of post doctoral training in an accredited program and subsequently obtain diplomate status from the American Board of Oral and Maxillofacial Pathology. The specialty focuses on the diagnosis, clinical management and investigation of diseases that affect the oral cavity and surrounding maxillofacial structures including but not limited to odontogenic, infectious, epithelial, salivary gland, bone and soft tissue pathologies. It also significantly intersects with the field of dental pathology. Although concerned with a broad variety of diseases of the oral cavity, they have roles distinct from otorhinolaryngologists ("ear, nose, and throat" specialists), and speech pathologists, the latter of which helps diagnose many neurological or neuromuscular conditions relevant to speech phonology or swallowing. Owing to the availability of the oral cavity to non-invasive examination, many conditions in the study of oral disease can be diagnosed, or at least suspected, from gross examination, but biopsies, cell smears, and other tissue analysis remain important diagnostic tools in oral pathology.[citation needed]
 An anatomical pathology instructor uses a microscope with multiple eyepieces to instruct students in diagnostic microscopy.
An anatomical pathology instructor uses a microscope with multiple eyepieces to instruct students in diagnostic microscopy.
Becoming a pathologist generally requires specialty-training after medical school, but individual nations vary some in the medical licensing required of pathologists. In the United States, pathologists are physicians (D.O. or M.D.) who have completed a four-year undergraduate program, four years of medical school training, and three to four years of postgraduate training in the form of a pathology residency. Training may be within two primary specialties, as recognized by the American Board of Pathology: anatomical pathology and clinical Pathology, each of which requires separate board certification. The American Osteopathic Board of Pathology also recognizes four primary specialties: anatomic pathology, dermatopathology, forensic pathology, and laboratory medicine. Pathologists may pursue specialised fellowship training within one or more subspecialties of either anatomical or clinical pathology. Some of these subspecialties permit additional board certification, while others do not.[23]
In the United Kingdom, pathologists are physicians licensed by the UK General Medical Council. The training to become a pathologist is under the oversight of the Royal College of Pathologists. After four to six years of undergraduate medical study, trainees proceed to a two-year foundation program. Full-time training in histopathology currently lasts between five and five and a half years and includes specialist training in surgical pathology, cytopathology, and autopsy pathology. It is also possible to take a Royal College of Pathologists diploma in forensic pathology, dermatopathology, or cytopathology, recognising additional specialist training and expertise and to get specialist accreditation in forensic pathology, pediatric pathology, and neuropathology. All postgraduate medical training and education in the UK is overseen by the General Medical Council.
In France, pathology is separated into two distinct specialties, anatomical pathology, and clinical pathology. Residencies for both lasts four years. Residency in anatomical pathology is open to physicians only, while clinical pathology is open to both physicians and pharmacists. At the end of the second year of clinical pathology residency, residents can choose between general clinical pathology and a specialization in one of the disciplines, but they can not practice anatomical pathology, nor can anatomical pathology residents practice clinical pathology''.[16][24]
COMMENTS FROM Dr. P. C. Majumder (- Author. Writer, Humanist, Physician (Physico-Mental & Spiritual) and Cosmopolitan Researcher in favor of ALL-CREATION Universally RESIDE++++ in positive ways for universal UNITY & LOVE++++) as follows:
1.
2.
3. 4. 5. 6. 7. 8. 8. 9. 10.
We're for all- ALL are for us for the greater interest of Humanism-Truth-Facts-Friendship-Unity-Participation to a Well-furnished GOAL of Truth from which all shall have ++++;
We're indebted to WIKIPEDIA +WHO for a short while and as 'Guardian QUOTATION' from Global WISER ONE. And have quoted many images, article's, writings etc. by great & humanist writers+++ from global thinkers, Well-wishers, Wiseman, Humanists and Others Living-Nonlivings in favor of HUMANISM to share more answers of Researchers-readers+++++....
To reach the 'GOAL of FULFILNESS' unitedly to alive in the "DESTINATION of TRUTH-FACTS-CHARMEST AMICABLITY" of Natural Joyful POSSIBILITIES+++
BREAST CANCER, TUMOR, Arsenic+Chemical Poisoning, Corona, Heart-Lung diseases, Neurological-Hormonal-Immunal-Infectious diseases with related complexities are possible to cure properly-easily-scientifically-accurately (100%) by our positive medical services only with+++++balance confirming
Medicine-Food control-proper nursing-medicinal massage-Medicinal Yogas- Meditation, Physiotherapy special etc. without side effects & Repeatation as per contract through user-friendly approved ways of CURE++++. please fill our form as below or click:
After confirming contract-letter between you+++. We serve you properly with no Chemo-therapy-radiation therapy -SURGICAL Complexities (Physical-Mental) to CURE+++ upto our Limit to recover your both-health from illness.